Welcome to our Monthly Journal Club! Each month I post a paper or two that I have read and find interesting. I use this as a forum for open discussion about the paper in question. Anyone can participate in the journal club, and provide comments/critiques on the paper by leaving a comment below. I picked this month’s paper because it demonstrates that toxic protein aggregates can spread from the gut to the brain, causing Parkinson’s disease-like symptoms. This is a major step forward for the ‘gut-brain’ hypothesis of Parkinson’s Disease, a really interesting idea that has gained a lot of traction (and hype) recently. This idea was first put forth by Heiko and Eva Braak, and is also referred to as the Braak Hypothesis. The paper we are discussing was published in Neuron, and is titled “Transneuronal propagation of pathologic alpha-synuclein from the gut to the brain models Parkinson’s Disease” by Han Seok Ko & colleagues at Johns Hopkins University in Baltimore.
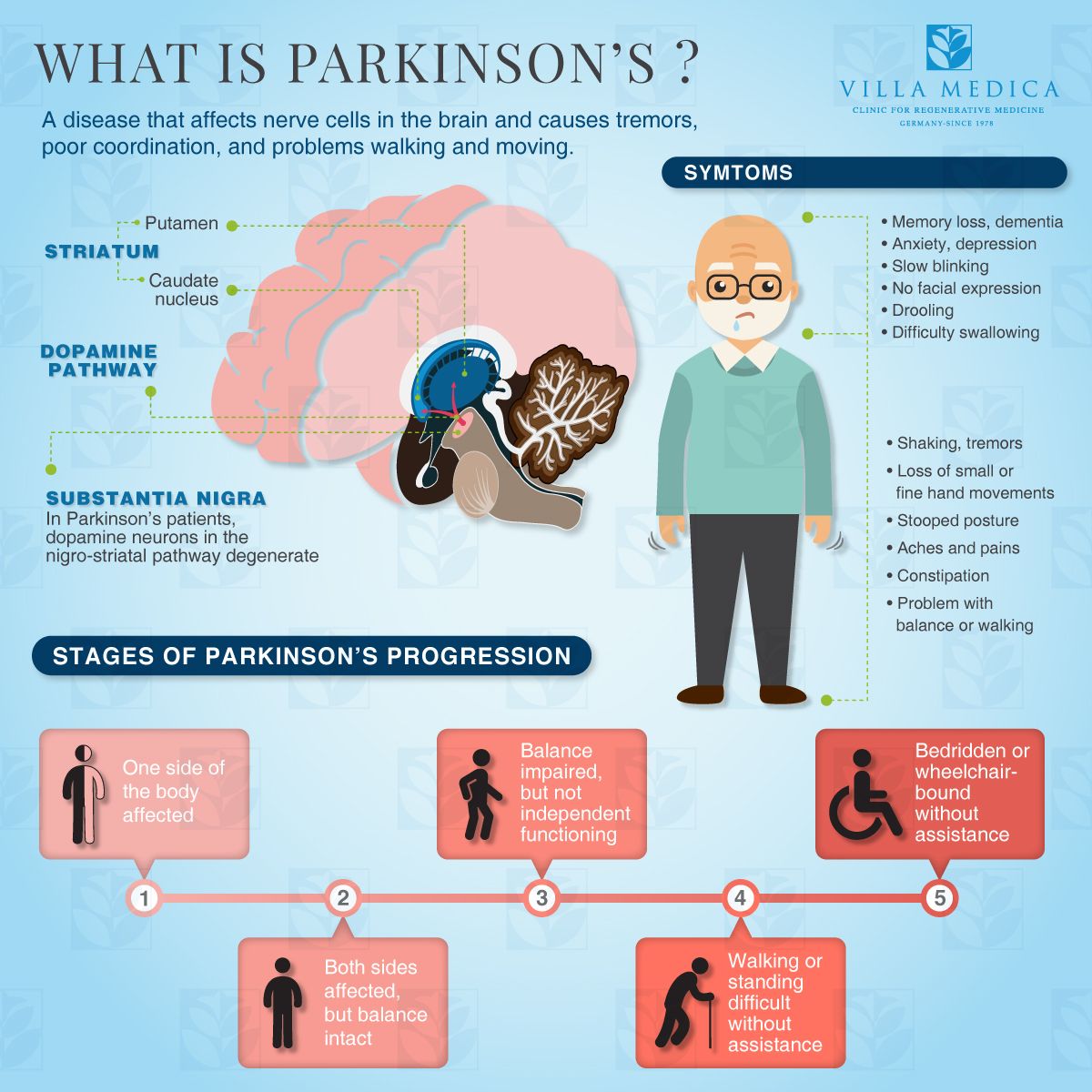
An overview of Parkinson’s Disease. (Credit: Villa Medica)
Parkinson’s Disease is a neurodegenerative disorder caused by destruction of dopamine-producing cells in the substantia nigra in the midbrain. The exact causes of this cell death are unclear, and several hypotheses have been tested and rejected time and time again (e.g., the autoimmune hypothesis). Parkinson’s Disease is part of a class of neurodegenerative diseases called ‘synucleinopathies’, which are characterized by aberrant aggregations of a protein called alpha-synuclein. Aggregates of this protein can be viewed in brain sections (using a microscope) and are termed ‘Lewy Bodies’. They spread throughout the brain in a characteristic pattern during the course of Parkinson’s disease, typically starting in the dorsal motor nucleus of the vagus (DMV) before reaching the midbrain. This suggests that problems may begin in downstream areas that relay signals through the DMV…like the gut. Whether alpha-synclein can travel from the gut to the brain has been a challenging question to answer. Using a clever approach, Ko & colleagues demonstrated that this is indeed possible when the protein is artificially induced into the stomach/small intestine area (see the figure below). A thing to keep in mind, however, is that this paper demonstrates that such a mechanism can exist, it doesn’t provide evidence that it does exist or ‘causes’ Parkinson’s disease in humans.
To cut a very long story short, others have shown that a pathogenic variant of alpha-synuclein can be made in a dish (in vitro), where they are termed ‘pre-formed fibrils; PFFs’. These fibrils can ‘jump’ from neuron-to-neuron in a living organism (in vivo) and cause symptoms remarkably similar to those found in sporadic Parkinson’s disease. The authors took advantage of these PFFs to test their hypothesis by injecting them into various parts of the gastrointestinal system, and seeing if they would ‘jump’ along nerve cells up to the brain, where they could promote the development of Parkinson’s disease.
Pre-formed Fibrils (PFFs) injected into the pyloric stomach (PS) or upper duodenum (UD) promote synucleinopathy in multiple brain regions. The pathology spreads in a stereotypical pattern resembling Parkinson’s disease progression. Alpha-synuclein aggregates are shown as ‘brown spots’ in the photomicrographs above. Note that mice receiving a control injection (PBS) do not show any aggregates even at 10 months post-injection (Credit: Kim et al., 2019).
After injecting PFFs into multiple areas around the gut (pylorus of the stomach) and upper small intestine (duodenum), they looked at the brains for signs of pathology at multiple time points (1, 3, 7, and 10 months). They observed aggregates of alpha-synuclein in multiple nuclei, showing a characteristic distribution pattern starting in the DMV and spreading all the way to the prefrontal cortex by 7-10 months post-injection. This is an exciting finding, as it demonstrates that pathological alpha-synuclein originating in the gut can promote Lewy body formation in the brain in as little as 1 month. The authors then asked whether these histological findings actually caused destruction of dopaminergic neurons in the midbrain, the neurodegenerative mechanism of Parkinson’s disease (see the figure below).
Injection of PFFs into the gut (pyloric stomach/duodenum) promotes the destruction of dopaminergic neurons in the mouse midbrain. Note the difference between the 7 and 10 month time-points between mice injected with PBS (control) or PFFs. Both dopaminergic (TH) and total (Nissl) neuron counts were drastically reduced by 7 months post-injection. Levels of TH, the dopamine transporter (DAT), and dopamine itself were significantly reduced by 7-10 months post-injection (Credit: Ko et al., 2019).
To examine dopamine-producing neurons in the midbrain, they stained brain sections using an antibody against tyrosine hydroxylase (TH), the rate-limiting enzyme in the dopamine production pathway. This protein is highly produced in dopamine producing neurons…so it can be used as a highly abundant and specific marker for these neurons. They observed drastic reductions in TH+ neurons (i.e., those that produce dopamine) in the midbrain 7-10 months following PFF injections into the gut! In addition to counting the number of TH+ neurons, the authors verified their data using a pan-neuronal marker (Nissl), another marker for dopaminergic neurons (the dopamine transporter (DAT)), and dopamine itself! All of these markers were reduced in mice that were administered intra-gastric PFFs.
Trucal vagotomy (TV) or knockout of endogenous alpha-synuclein (Snca-/-) prevents the destruction of midbrian dopamine neurons characteristic of Parkinson’s disease! Note that alpha-synuclein aggregates (p-alpha-Syn; green color) were only observed in mice with intact vagal nerves and with normal copies of the Snca gene (Credit: Ko et al., 2019).
The next logical step is to see whether blocking transport of PFFs into the brain, or knockout of alpha-synuclein altogether, can prevent these pathologies from developing. To block the transport of these toxic proteins, the authors cut a portion of the vagus nerve (truncal vagotomy; TV), the neural superhighway connecting the body to the brain. When they repeated their experiments in mice that underwent the TV procedure, they no longer showed signs of Parkinson’s disease (Lewy bodies or loss of dopaminergic neurons)! This strongly suggests that PFFs travel via the vagus nerve (across multiple synapses!) from the gut to the brain, where they promote the destruction of dopamine-producing neurons (see the figure above). Another hypothesis to the ‘jumping’ idea mentioned above is that PFFs seeded in the gut promote the misfolding of normal alpha-synuclein, which then propagates to the brain. If this is the case, then knocking out normal alpha-synuclein (the gene is called Snca) would also prevent the development of Parkinson’s disease, as the toxic PFFs wouldn’t be able to promote the misfolding of alpha-synuclein which cause disease.
When the authors repeated their experiment in mice lacking the gene for alpha-synuclein (Snca-/-), they observed no destruction of midbrain dopamine neurons, just like in mice whose vagus nerves had been cut! This additional experiment supports the idea that PFFs can cause a cascading spread of misfolded alpha-synuclein which ultimately reaches the brain to cause disease!
The authors went onto test whether injection of PFFs into the gut causes Parkinson’s disease-like symptoms (in addition to the brain pathology), and whether TV or knocking out Snca could prevent these behavioral problems. Using a battery of behavioral tests, they demonstrated that gut-injections of PFF cause mice to develop balance problems, memory impairments, reduced strength, olfactory (smell) deficits, and impaired cognition. Importantly, they observed that TV or Snca ablation rescued these behavioral problems that closely resemble Parkinson’s disease (data not shown here; see the primary paper linked in the first paragraph).
Summary of the study’s findings. In a ‘normal’ mouse, injection of pre-formed fibrils into the gut causes Parkinson’s disease-like symptoms and pathology. This can be prevented by cutting the vagus nerve or by knocking out the gene for alpha-synuclein (Snca-/-) (Credit: Ko et al., 2019).
This study provides exciting support for the Braak hypothesis, and suggests that pathogenic alpha-synuclein in the gut can cause the misfolding of the endogenous protein, which then propagates to the brain via the vagus nerve to cause Parkinson’s disease-like symptoms and pathology. Whether this phenomenon occurs in humans is still an open question. If it does, a whole new class of therapeutics for Parkinson’s disease targeting the gut/nerve interface could be around the corner! I can’t wait to see what comes of this research going forward! So now its your turn to tell me what you think by leaving a comment below or by tweeting at me on twitter! See you next time guys…and as always…stay curious!